What is Benign Prostatic Hyperplasia (BPH)?
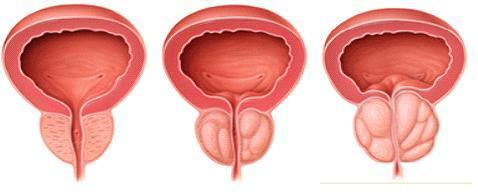
Benign Prostatic Hyperplasia (BPH or BPE) is a normal part of the ageing process that can affect men by the prostate enlarging. This is brought about by the cells in the prostate dividing more quickly causing the prostate tissue to grow or enlarge. A small amount of prostate enlargement is present in many men over the age of 40 and particularly affects men over the age of 50. Nearly half (43%) of men over the age of 65 have either some urinary symptoms or a reduced urinary flow due to BPH. As many as 9 out of 10 men in their seventies and eighties have some symptoms of BPH.
BPH is characterised by the non-cancerous (benign) growth of prostate cells, with the effect that the middle portion of the prostate progressively enlarges. The part of the urethra (water pipe that takes urine from the bladder to be expelled from the body) that runs through the middle of the prostate can become squeezed. As a result the flow of urine is reduced and the man finds that his urine stream becomes weak, dribbly and it is more difficult to empty his bladder often causing discomfort.
Because urine flow is restricted, your bladder has to work harder to push urine out leading to the bladder walls becoming thickened and less stretchy. So the bladder cannot store as much urine. These are called the ‘storage symptoms’ (frequency, urgency, nocturia) and are often the symptoms that are most troublesome and are usually the reason for men seeing their GP.
If symptoms seem to be getting worse, it is usually due to how much the enlarging prostate tissue is squeezing the urethra rather than how much your prostate is enlarging.
It may be reassuring to know that BPH is neither connected with prostate cancer nor does it mean there is an increased risk of developing prostate cancer, but it can cause worrying symptoms.
For publications with more information on BPH please see our resources.
Symptoms
There are a number of symptoms of BPH. In all probability, you won’t experience of all of these symptoms. The most common symptoms are:
- Poor stream – the urine flow is weaker and it takes longer to empty the bladder;
- Intermittent stream – stopping and starting when passing urine;
- Straining – having to push to get urine to start to flow;
- Hesitancy – having to wait for a while before urine starts to flow;
- Dribbling – after finishing, a bit more urine may trickle out and stain underpants;
- Frequency – having to pass urine more often;
- Getting up several times a night, every night to pass urine is common and is called ‘nocturia’;
- Urgency to pass urine – having to get to the toilet fast;
- Poor emptying – a feeling of not quite emptying the bladder.
There is a symptom self-test that will help you and your doctor understand the severity of your symptoms. It will not give a diagnosis.
Usually the symptoms are mild to begin with – perhaps a slight reduction in flow of urine or having to wait a few seconds to start passing urine. As the years go by, symptoms may become more troublesome. Sometimes BPH can also lead to kidney problems through the pressure that can be created in the kidneys, due to the bladder not being able to empty.
It is important to tell your doctor about urinary problems such as those listed above although it is important to note that these symptoms may be related to other diseases such as kidney problems or urinary tract infections. If you did the symptom self-test you can print it out and take it along to give the doctor a good idea of your difficulties. In 8 out of 10 cases, these symptoms suggest BPH but can also signal another prostate disease such as prostatitis or prostate cancer.
This is why it is important to see your GP sooner rather than later as further tests may be necessary before a final diagnosis can be made. The earlier that a diagnosis is made and treatment, if any is necessary started, the better the outcome is likely to be.
In some people, the symptoms become quite severe and a complete blockage of urine may develop (‘retention of urine’), needing urgent treatment.
Risk factors
The incidence of BPH tends to increase with age. It particularly affects men over the age of 50 and nearly half (43%) of men over the age of 65 have either urinary symptoms or a reduced urinary flow due to BPH. As many as 9 out of 10 men in their seventies and eighties have some symptoms of BPH.
The size of the prostate does not always determine the severity of obstruction or symptoms. Some men with greatly enlarged prostate glands have little obstruction and few symptoms, whilst others with a less enlarged prostate have greater problems, although generally the larger the prostate the greater the risk. However, you may not know that you have any obstruction until you suddenly find yourself unable to urinate at all. Although not common, this condition is called acute urinary retention.
Severe BPH can lead to urinary tract infections, bladder or kidney damage, bladder stones and incontinence – the inability to control urination. If the bladder is permanently damaged, treatment for BPH may be ineffective. When BPH is found in its earlier stages, there is a lower risk of developing such complications.

Investigations and tests
Urine Sample
Your doctor may wish you to provide a urine sample to check if you have blood in your urine, glucose and for any signs of infection in your bladder or kidneys.
Blood tests
PSA blood test Prostate Specific Antigen (PSA test)
PSA is a protein made in your prostate and it is normal for small amounts of PSA to leak out of the prostate into your bloodstream. As you get older, or if your prostate is damaged or enlarged (such as with BPH) then more PSA can leak out into your blood giving a higher PSA level. Therefore your GP may want to do a PSA blood test to check for potential problems with your prostate and may explain more to you about the PSA test and what the results might mean.
Another blood test that your doctor might do is to check for kidney problems by testing for a substance called creatinine, which is present in the kidneys.
Digital rectal examination (DRE)
A DRE involves the doctor sliding a gloved finger into the back passage to check the prostate; it gives the doctor an idea of the shape, size, if there are any hardened areas or lumps and the general condition of the prostate. Although it might be a bit uncomfortable, it shouldn’t hurt and only takes a few minutes to do but will give the doctor a much better idea of what is going on .
If you prefer, you should be able to request an appointment with a male doctor when you book your appointment
Voiding diary
Your GP may ask you to keep a ‘voiding’ diary. (Voiding means passing urine.) The GP may ask you to keep a record of or be aware of such things as; the number of times you pass urine during the day, the number of times you get up during the night to pass urine if there is an urgency when you need to pass urine. To do this, you may find the recording form ‘visits to the toilet diary’ helpful. It may also be helpful if you undertake the symptom self-test and print a copy of the results before you go to see the GP.
Tests which the urologist may undertake
Your GP may decide that you need to be seen by a doctor in hospital who specialises in treatment of the prostate called a urologist.
Urine Flow measurement
The urologist may ask you to attend for a urine flow measurement to check how quickly/slowly you are passing urine. For this all that you have to do is pass urine into a special device that measures how quickly the urine is flowing. A reduction in urinary flow is often associated with prostate enlargement.
Ultrasound scan
The doctor or radiographer runs a small probe that emits ultrasound waves over the surface of your tummy. This is to look at your kidneys but can also measure how well your bladder is emptying and gives a picture of your bladder and prostate.
Trans Rectal Ultrasound Scan
In some cases, in order to get a better picture of the prostate, you may be asked to have a trans-rectal ultrasound scan. A small probe is slipped into the back passage to direct the sound waves to the prostate. The echoes from the sound waves give a clear picture of the shape and size of the prostate on a screen.
Cystoscopy
To examine the bladder and urethra, a thin, flexible tube which has a camera on the end is gently passed up through your penis into the urethra and images from the camera show the bladder and urethra on a screen. The examination should only take about 5-10minutes. Afterwards you may feel a bit sore or have a burning feeling when passing urine and you may notice be a little blood in your urine for a few days.

Treatments
There are three different types of treatment:
- Lifestyle change with monitoring;
- Medication;
- Surgical procedures
Treatments for BPH aim to help with the symptoms but don’t deal with the cause of or cure BPH no matter which treatment you are advised to have. For further information see the BPH and treatments-explained and the Spotlight on treatment for an enlarged prostate;
Lifestyle change with monitoring
Unless symptoms are troubling, your GP, urologist or CNS may decide on lifestyle change with monitoring in the first instance.
When might this be suggested?
If your symptoms are not troubling you too much and you’re happy to live with the symptoms as they are, your doctor may decide on giving you healthy lifestyle advice and keeping an eye on how you are.
What lifestyle change advice can I expect?
- Avoid drinks for a few hours before going to bed;
- Limit your intake of drinks containing alcohol and caffeine. Caffeine is found in tea, coffee and cola drinks. Remember energy and performance drinks or energy shots can have high amounts of caffeine added;
- Avoid drinking large quantities of fluid at any one time;
- Exercise regularly. Try walking for about 30 minutes (or more) every day as this can improve symptoms. If you haven’t exercised for a long time you should build this up gradually and check with you GP before starting to exercise;
- Eat a healthy diet. If you are very overweight try to shed those extra pounds by cutting out sugar and sugary foods, fatty foods and takeaways. If you need help with losing weight, ask if you can be referred to a weight loss clinic;
- Stop smoking. This is good advice for your general health;
- Learn to relax if you can and have less stress in your life
- Make notes about any new symptoms, or if your symptoms are getting worse, and let your doctor know
What does monitoring involve?
You will have a regular check-up with your GP or urologist who will monitor your symptoms to see if they are staying the same or getting worse.
As part of the monitoring process you may have your urine tested or blood taken to check your PSA level.
Are there any side-effects?
As there is no active treatment, you should not experience any side-effects and hopefully you may notice an improvement in symptoms.
What happens next?
If you find that symptoms have been getting worse and affecting your quality of life, then your doctor may suggest that you begin medication to help deal with the symptoms of BPH. Although medication may not be suitable for all men
Medication
In some cases medication(s) may be prescribed to help deal with the symptoms of BPH although medication may not be suitable for all men. There are 2 types of medication that can be used; inhibitors and blockers.
Surgery
Surgery is considered the most effective treatment for BPH and is used in men with severe symptoms that persist after other treatments have been tried. There are a few different types of surgery available nowadays including :
- Trans Urethral Resection of the Prostate (TURP)
- Trans Urethral Incision of the Prostate (TUIP)
- Green Light Laser (GLL)
- Holmium Enucleation of the Prostate (HoLEP)
For more information please see the guide: Spotlight on treatment for an enlarged prostate
General advice that may help with symptoms
Drinks
- Don’t drink too much before bedtime and in fact it may be wise to stop taking any fluids for a few hours before going to bed to help reduce night time trips to the toilet;
- Limit alcohol intake as alcohol can irritate the bladder making you pass urine more often;
- Cut down on caffeine. Caffeine is found in tea, coffee and cola drinks and can increase the amount of urine your body produces. Energy and performance drinks or energy shots can have a high amount of caffeine added.
Weight
If you are very overweight, it may help with symptoms if you lose some weight. If this is the case, start by trying to have a healthier diet and cutting down or cutting out sugar, sugary foods, sweets, chocolate, fatty or fried foods, crisps, chips or takeaways.
Smoking
Although smoking doesn’t cause prostate disease directly it is linked with many other illnesses. If you are going for a surgical procedure smoking increases risks for you.
Keeping active
Try to have some moderate physical exercise at least five times a week. This could be as easy as walking for 30 minutes every day. If you haven’t been used to exercising before then build up gradually until you are able to walk for 30 minutes without being out of breath. When seeing your GP you can check about starting to exercise.
Check your medicine cabinet
Some medicines can make your symptoms worse as they can affect your bladder, making it more difficult to pass urine. These include over-the-counter cold relief medicines and antihistamines. Ask the pharmacist for more advice if you have any doubts.
Passing urine
Go to the toilet to pass urine as soon as you feel the need. Waiting can stretch the bladder and cause more problems. It also may be helpful to go to the toilet whenever you have the chance as this may help cut down on the times when you feel the need to get to the toilet urgently.
Try what doctors call ‘double voiding’. (Voiding just means passing urine) When you think you’re finished try going again to help make sure your bladder is empty.
Over-the-counter medicines
There is a medicine that can be bought over-the-counter at pharmacies to help with symptoms of BPH called ‘Flomax Relief ®’. This contains tamsulosin. Before being able to purchase Flomax Relief®, the pharmacist will take you through a short questionnaire asking about your symptoms to make sure that Flomax Relief ®is the right treatment in your particular circumstances. If it is decided that this may be beneficial then the pharmacist will supply a 2 week course of Flomax Relief® with a review of symptoms and side-effects after the 2 weeks.
If it has helped, then Flomax Relief may be supplied for an additional 4 weeks. An appointment should be made to see your GP within this 6 week period to discuss your symptoms and any further treatment.
Herbal supplements
A brief word about Saw Palmetto
You may see advertisements for saw palmetto remedies as a treatment for symptoms of BPH. The berries of this plant are used in herbal remedies. A number of studies have suggested that saw palmetto helps to relieve some of the symptoms of BPH; such as having to pass urine frequently, during the night or difficulty in passing urine. It would seem that some men find a mild improvement of these symptoms when taking saw palmetto.
Herbal remedies such as saw palmetto are not suitable for everyone so chat this over with your GP before you take them. If you decide to go ahead with saw palmetto then let your GP, urologist, clinical nurse specialist (CNS) or pharmacist know that you are taking this herbal remedy.
Studies have been undertaken to find out how this might affect the PSA level. Although these studies seem to suggest that saw palmetto does not affect PSA levels, some doctors suggest that if you are having any difficulties with passing urine you might consider having a PSA test before starting saw palmetto just to be on the safe side.
What the medical words mean, abbreviations that you might hear and medical staff that you might meet.
When you have been diagnosed with any disease or condition, unavoidably, there will medical words and abbreviations that doctors, nurses and other medical staff will use that you have never heard of and will perhaps not know what they mean and prostate disease and prostate cancer are no different.
A helpful list of terms you might come across is provided here in alphabetical order.